80M with SOB, body pains and lower backache
Case of 80yr old male with shortness of breath, body pains and lower backache
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CHIEF COMPLAINTS
A 80yr old male came to the opd with shortness of breath since 4 months, body pain since 4 months and lower backache (right side) since 6 months
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic 6 months ago then he developed lower backache on right side since 6 months
Insidious in onset and gradually progressive in nature, dragging type of pain, intermittent in nature, aggravated on walking and relieved on rest. Shortness of breath since 6 months which is present on ordinary and less than ordinary activity , grade (2-3) relieved on rest.
No C/O chest pain, orthopnea, PMD,decreased urine output, pedal edema or facial puffiness. Generalised body pains 4 months.
PAST HISTORY
Not a known case of hypertension, DM, CVA,CAD,TB, asthma.
20 yrs back he had cataract surgery for his right eye and 15 yrs back he had the same for his left eye.
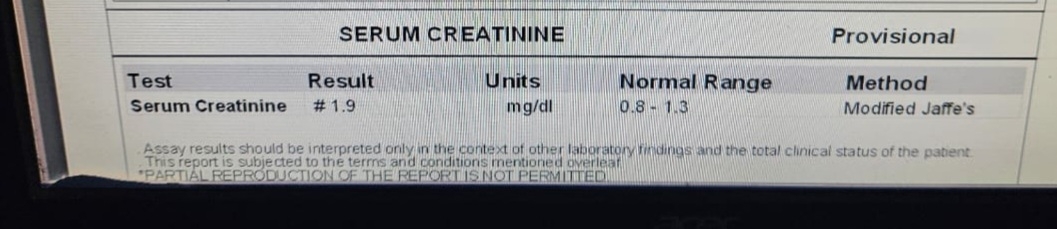
3 yrs back he met with an accident and had tibial fracture and was taken to local hospital for treatment where he was also diagnosed with CKD.
1yr back when he went for the removal of the rods in his leg he had an infection with swelling of his foot.
6 days back he had chest pain radiating towards right for which he went to RMP and was given a pill which gave him relief.
FAMILY HISTORY
No significant family history
PERSONAL HISTORY
Alcohol and smoking bedi since 28yrs
GENERAL EXAMINATION
Pallor positive
No signs of icterus, cyanosis, clubbing, lymphadenopathy and pedal edema.
PR: 89bpm
BP: 130/70mm hg
RR: 22 bpm
TEMPERATURE: 98.6F
SYSTEMIC EXAMINATION
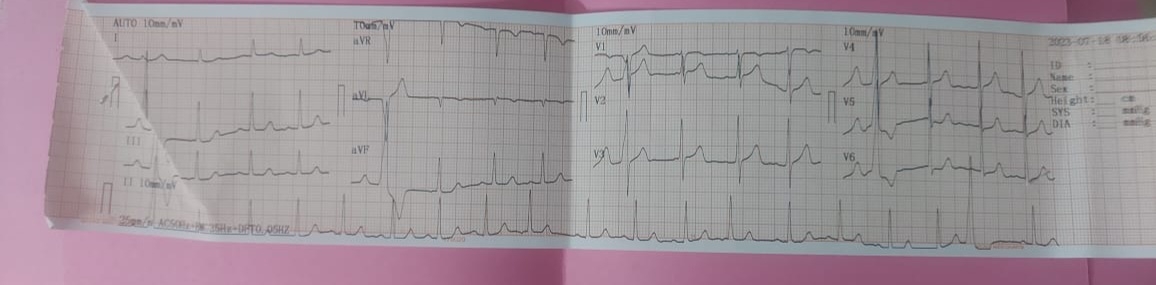
CARDIOVASCULAR SYSTEM:
S1 S2 heard
no murmurs
RESPIRATORY SYSTEM:
No added sounds
ABDOMEN EXAMINATION:
Shape: scaphoid
No tenderness, palpable or free fluid
Liver and spleen not palpable
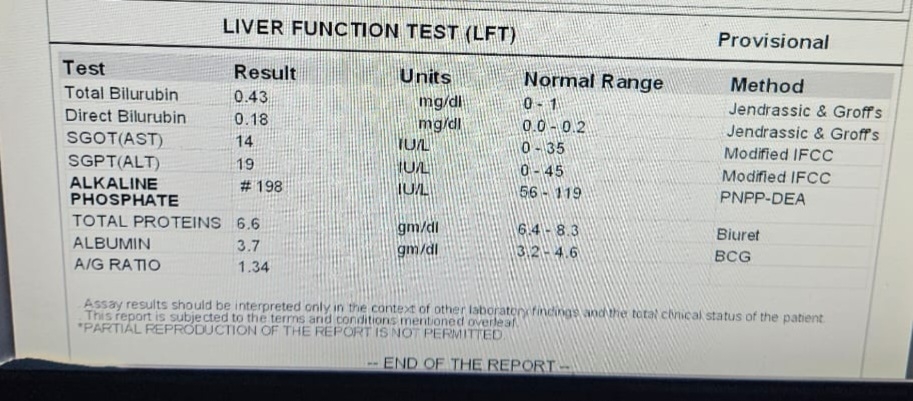
INVESTIGATIONS














Comments
Post a Comment